Four years of studying eyeballs: how to organize information
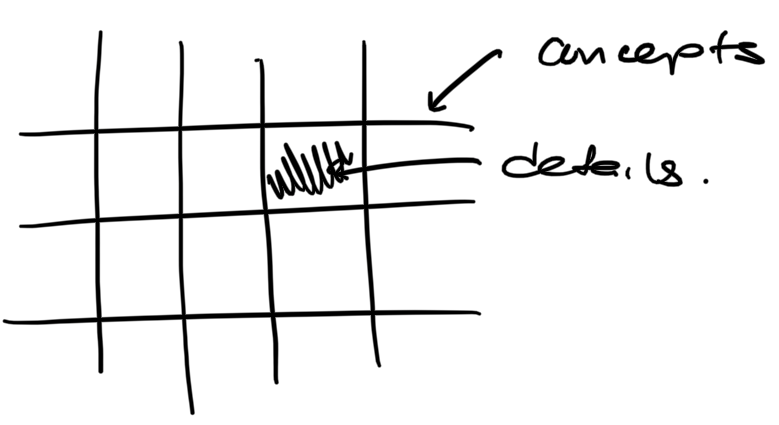
I think that learning something is divided into two main parts - understanding concepts, and memorizing details. I picture it in my head like this:
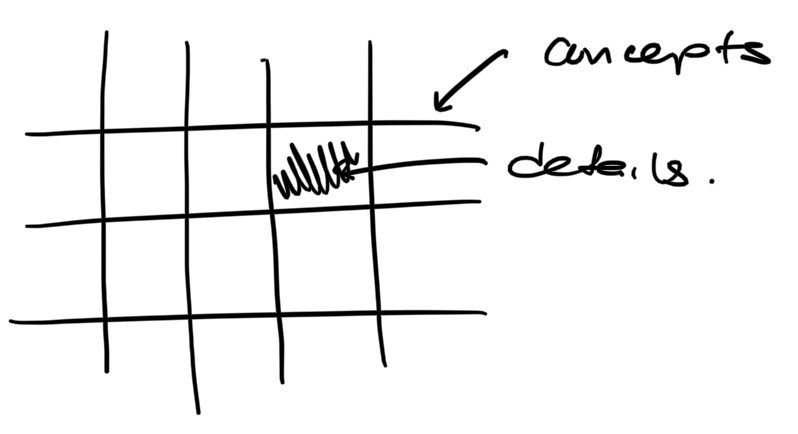
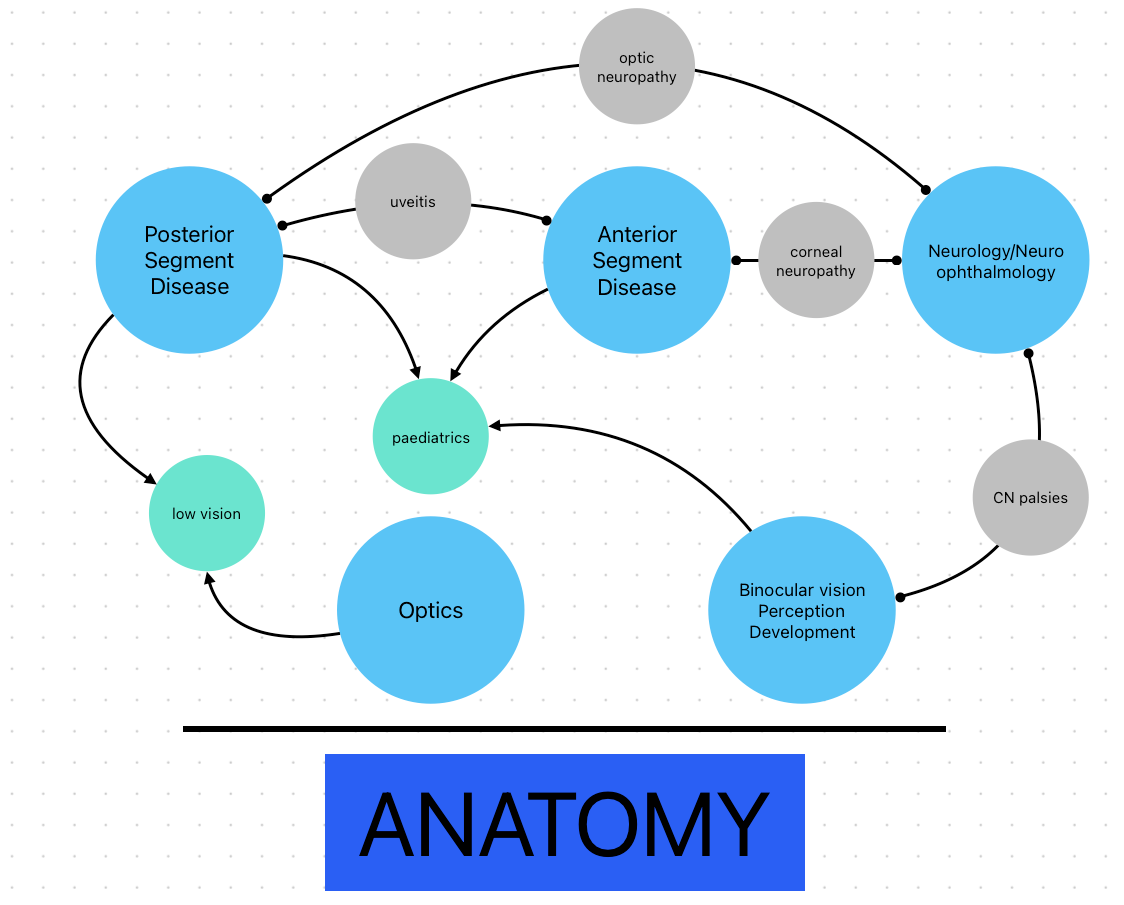
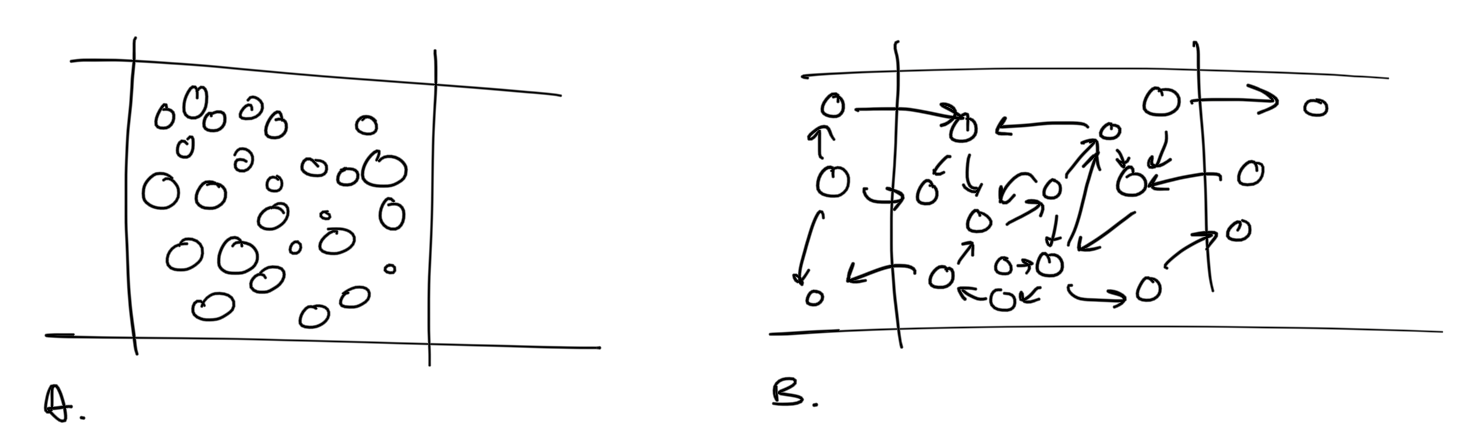
Concepts give us the framework upon which we can fill in the details. Different subjects and topics have a different structure and ratio of concepts to details. For example, physics relies mostly on concepts, and there are relatively few details to memorize. My mental picture of physics looks like this (A).
Other topics, like biology, look more like B - fewer concepts, and more details to memorize and remember. My approach to studying is to always understand the concepts first, and fill in the details later. Concepts provide critical context and structure to the details, and serve as the organizational matrix for facts to sit in my brain.
The nature of clinical medicine and education is that there’s a lot of information to cover, and it’s driven by a lot of broad stroke, big picture data. Clinical knowledge do not always have logic or structure, and in some ways, it’s not important in the context of clinical practice - at baseline, it’s unnecessary to know how or why a certain treatment works, only that it does. Knowing how a certain disease came to be is less important than what it looks like and what to do about it.
Optometry school, an institution for clinical education, parrots this approach. There were tons and tons of facts and details to memorize, but few concepts to organize them with. The bars of conceptual structure were set so far apart that I could not see them, and I felt like I was drowning in the sheer amount of factual, decontextualized information I had to download and regurgitate.
Sink or swim, right? I took on the challenge, and went ahead shoving these facts into my brain. It was an unpleasant, academically unstimulating process, but it allowed me to do well on tests. The issue did not show up until third year, when I began to see patients. At this stage, I realized that while this information was great for vomiting onto a test paper, I had no idea how to apply it in the real world. I had only storage boxes full of disjointed pieces of knowledge that remained largely unconnected. I had a patient once with recent onset double vision only present when both her eyes were open. I knew from my neurological disease box that this might be some sort of cranial nerve issue. I knew from my binocular vision box that the cover test could be used to gather information about an eye turn. But my overly compartmentalized brain did not make the connection to apply binocular vision testing to neurological disease, because neurological disease is neurological disease, and binocular vision is binocular vision, and binocular vision is never neurological disease.
Four months later, in the second term of my third year, I started studying for my NBEO board exam. Things started to come together and I came up with a more fun, more applicable way to study.
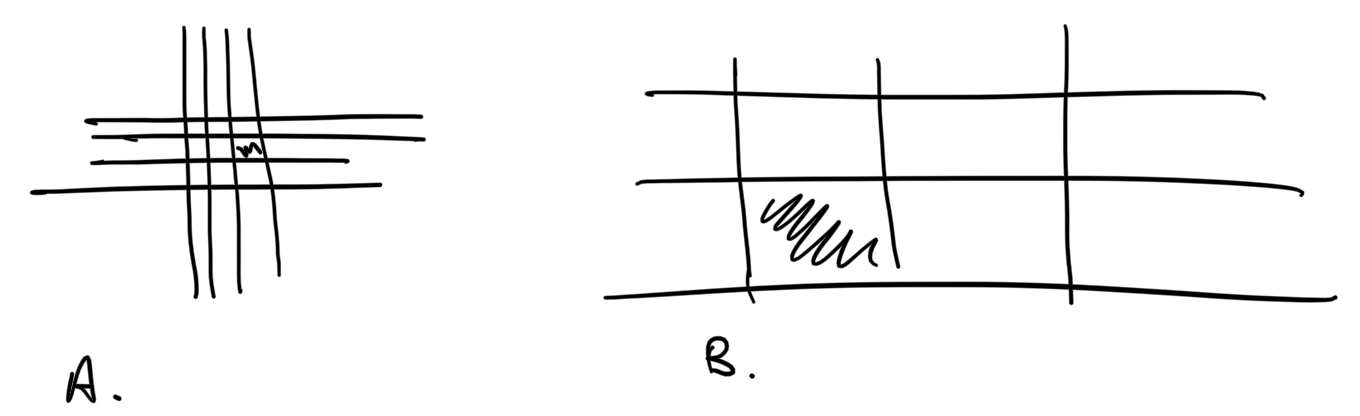
I started to look at optometry as being split into five main categories: posterior segment disease, that is, issues at the back of the eye, including retinal disorders like macular degeneration. Anterior segment disease - diseases of the front of the eye, like keratoconus. Binocular vision/development and perception. Neurology and neuro-ophthalmology. And optics. The foundation for all these topics is anatomy. Topics such as paediatrics and low vision I started to see as combinations and intersections of the other categories. For example, much of paediatrics is binocular vision/development and disease. Much of low vision is posterior segment and optics.
With this big picture in mind, I started to build my grid. I think the retina is cool, so I started there. Posterior segment diseases would make little sense without the underlying anatomy. So I started constructing a skeleton with a general overview of the anatomy of the retina. What do the layers look like? Where does it get its blood from? I made sure to make this brief - I just wanted a general idea of what was going on. And then I started with a disease - what it was in broad strokes, then in terms of its pathophysiology. OK. Diabetic retinopathy. Eye disease, happens when sugars are too high in the blood. Can cause vision loss. Caused by damage to pericytes due to elevated blood glucose. When I didn’t know something about the anatomy or physiology pertinent to a disease, I’d circle back to anatomy and fill in the details there. What do pericytes do? They take care of small blood vessels. No pericytes? Damaged blood vessels. Loss of blood-retinal barrier. What does this cause? Bleeding and leakage. OK. Cool. What happens then? Retina can’t get enough oxygen. So what? It tries to make more blood vessels to get more oxygen. How? Releases vascular endothelial growth factor. What else happens? Parts of the retina start to swell and die. What is this called? Cotton wool spots. In this way, I would create a story to link together all the facts I had to know. Now, instead of a list, I had a web.
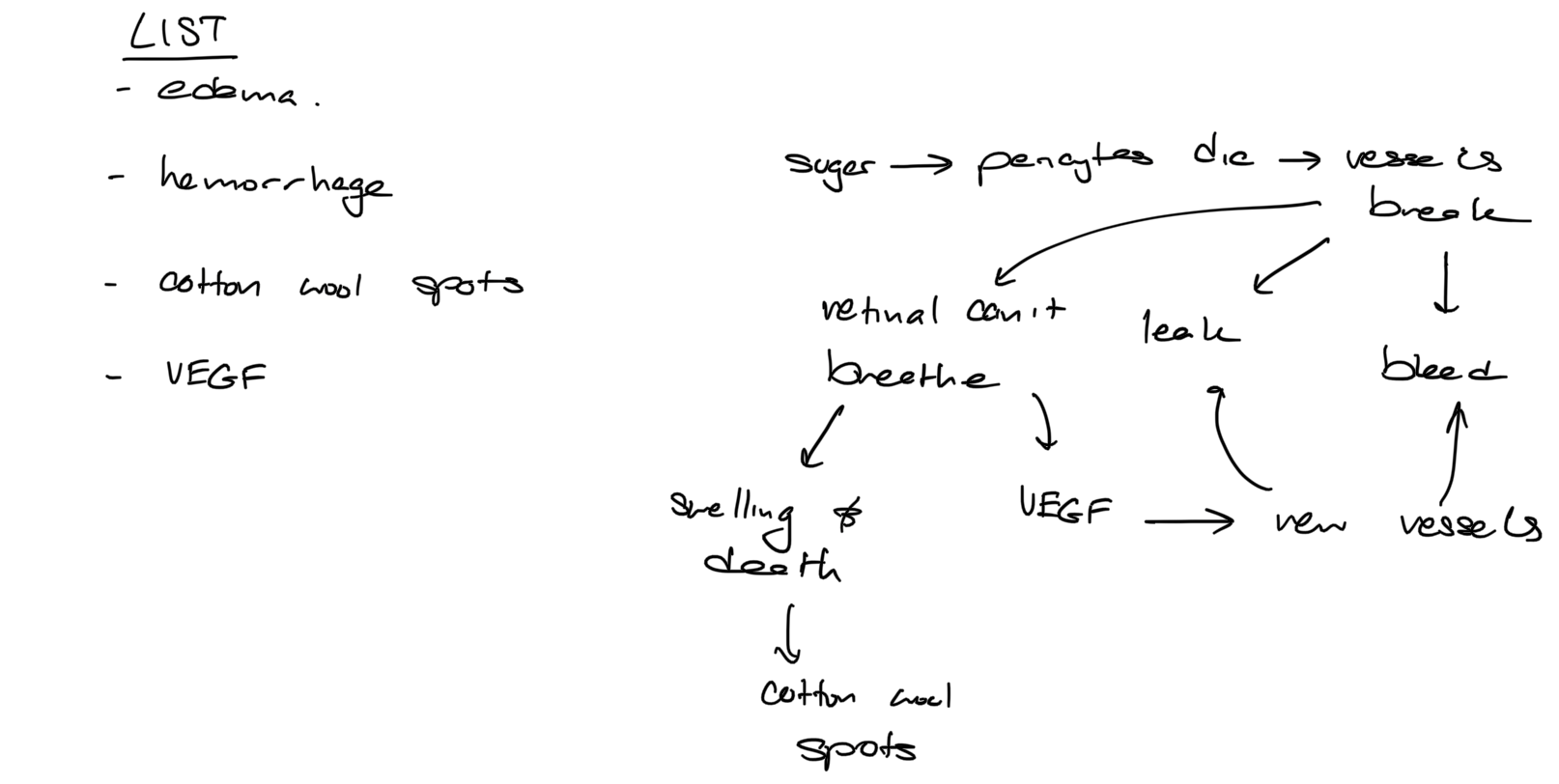
Facts are disposable, but concepts are reusable. To know that diabetic retinopathy presents with oedema and hemorrhage only tells me about diabetic retinopathy. And so I tried to extricate some concepts and patterns from what I had learned. Here, I can see that blood vessel damage leads to bleeding, leaking and retinal hypoxia. Retinal hypoxia causes the formation of new vessels which also leak and break. Could this happen anywhere else? And so I learned about my next condition. Central retinal vein occlusion. Retinal vein drains the whole retina. It gets blocked. What happens? Vessel damage. I know from my DR story that vessel damage can cause leaking, bleeding and new vessel formation. Is the same idea applicable here? Lo and behold, we see those exact things in CRVO.
In the same way, while building up my network I would try to make as many connections as I could at a more macro level. Looking at our categories, I came up with examples like the following. Like we talked about earlier, neurology and binocular vision are connected by palsies of cranial nerves controlling extra ocular muscles. Neurology and posterior segment disease are connected by optic nerve conditions. Anterior and posterior segment disease by uveitis. Neurology and anterior segment disease by corneal neuropathy.
And so within the skeleton of anatomy (pun intended), I’d build an understanding of disease. By making connections within and between diseases, I’d create a context, a network upon which I could organize my facts. Learning in this way, emphasizing understanding and connections, made studying much more fun, and allowed me to get past my mind block of boxes.
Zooming in on the grid, it originally looked like this (A). Studying by focusing on connections made it look like this. (B)
I’m in the last term of my fourth year now, and most of my learning is taking place through real world patient interactions, outside of textbooks. Even so, I find this model to be applicable, I’m continuing trying my best to cultivate my knowledge network as much as I can to be the best clinician I be.
I hope the contents of this post gave you something to think about. Happy studying! Thanks for reading.

Member discussion